Helping Payers - Both, Private & State Plans
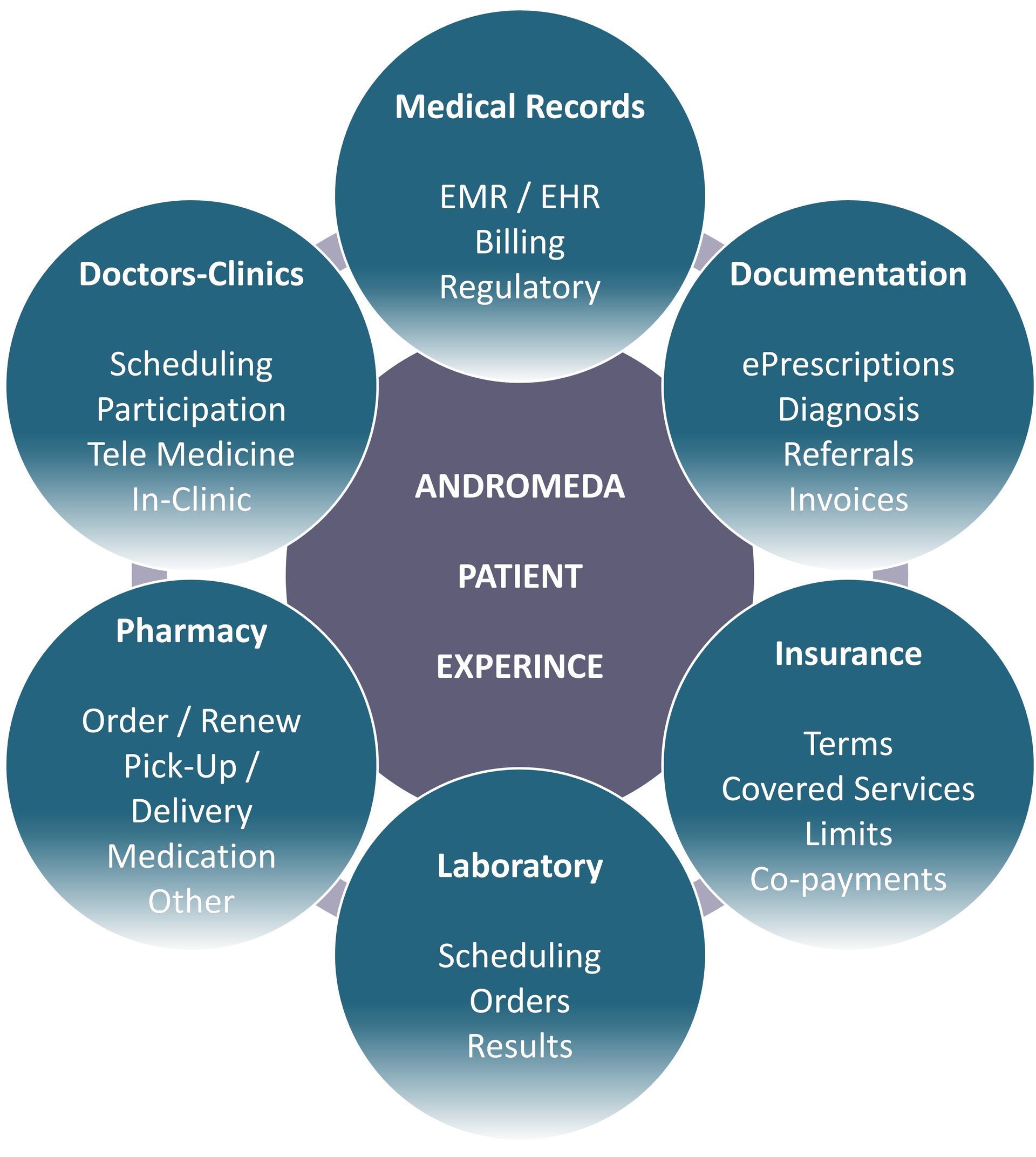
Our platform helps payers / insurance companies organizing the following processes more efficiently at a large scale: payer-provider inter-operability, full enhanced eligibility inquiry, screening programs & early detection of risk groups, patient relationship, medical documentation and their review, billing & claims processing, equity & transparency, policy sales. As a result, quality of service improves, client satisfaction increases and overhead costs decline. While we enhance the patient journey and make it seamless, we help Payers keep the claims ratio / loss ratio low. Platform allows automating processes that are currently mostly manual and human-based, therefore minimizing margin of error.
Payer (Insurance) Value Propositions
Equity & Accessibility
Improved Efficiency
Reduced Errors
Patient Satisfaction
Engagement & Conversion Ratios Grow by 10%-30%
Claims Overhead Costs Reduce By 35%
Instantaneous, Real-Time Access To Medical Claims
NPS / CAHPS Improve by 10-30 Points
We Bring Efficiency, Inter-Operability & Power Analytics
You Capitalize On Improved Service Quality And Reduced Costs
Improved Inter-Operability, Patient Service Quality & Reduced Costs
We connect everyone in the healthcare ecosystem, automate support & administrative processes and allow payers / insurance companies (both, private and state plans) to:
- Digitalize and automate full eligibility inquiry at admissions, opening medical case / claims and their review
- Have instantaneous access to each medical case and claim, upon its very inception and follow it online, in real-time
- Start claims processing & analysis earlier, when the event originates, and follow it in real-time vs having the same information at a conventional weekly or monthly billing cycles, post-factum, when the case is completed
- Reduce average review time per medical case / claim
- Significantly reduce workload on call centers and back office
- Reduce claims processing overhead & administrative costs
- Obtain full analytics on medical cases, billing and claims, to improve claims ratio and improve provider relationship
- Reallocate released time & resources on sales and underwriting
- Reach out patients / subscribers directly, through pushing follow-up meetings in the system, or through direct messenger communication or direct in-app video communication
- Enhance screening programs to allow early detection, lowering clinical risks and treatment costs
- Reduce claims ratio / loss ratio
Shorter Medical Case Access Time & Claims Review Time
- Instantaneous, real-time access to medical cases
- Full digital review of medica cases
- Real-time, digital approval of pre-authorizations
- Shorter time needed for claims review and processing
- No time required on analytics
Significantly Improved Client / Patient Satisfaction
- Uninterrupted and seamless user journey
- Super convenient and easy-to-operate user interface
- Transparent environment with best-in-class search and compare features
- NPS / CAHPS significant growth
Securely Storing & Reviewing
Documentation
- Medical records
- Lab test results
- Radiology results (images)
- Insurance documentation: insurance policy & plan details, provider lists, services & tariffs, minimal spend & co-pays, pre-authorizations, approved or rejected claims, etc.
- Billing documentation: invoices, paychecks, etc.
Financials, Costs & Revenues
- Increased private insurance sales and Medicaid premiums due to increased NPS / CAHPS
- Decreased claims ratio / loss ratio due to reduced human errors and early access to medical cases
- Free online brokerage: lifetime, no-fee sale of insurance policies in the platform & app
- Reduced overhead costs on billing processing, claims processing, patient interaction and policy sales
Electronic Workflow, Pre-Authorizations & Claims
- Automatic approval of standard pre-authorizations
- Instantaneous review and approval of non-standard pre-authorizations
- Online, real-time review of prescriptions, referrals, medical case
- Telemedicine integrated
- In-app interaction with patients
- Online review and approval of claims and refund requests
Prescriptions, Medications
In-Store Eligibility Inquiry
- Enhanced eligibility and plan inquiry inside pharmacies & drug stores
- Access patients' ePrescriptions and there adherence reports
- Unique medication substitution algorithms
- Fully automated monitoring of adverse drug reactions & adverse drug events
For More Information and Demonstration
Inquire Today
Thank you for contacting us.
We will get back to you as soon as possible.
Please try again later